Security lapse occurred on June 12, 2008, at street entrance to National Book store at Robinsons Ermita. The person at said entrance didn't inspect two compartments of my waist bag. Said compartments were large enough to contain deadly weapons. The exit of said store leads to said mall. From said store, I was able to proceed to other parts of said mall. Nobody in said mall inspected said bag.
customer advisory re Philippine Star newspaper and magazine
For their own benefit, it will be advantageous for customers to not follow recommendations for products or services wherein the complete name of the source(s) and complete address(s) of the source(s) of said recommendation(s) is not
clearly visible in the same location wherin said recoomendation is published. An e-mail address is not acceptable. If customers follow recommendations in said publications for products, services, and persons who render said services and the said recommended products and services are unsatisfactory, said customers will not know whom to hold responsible. Similarly, it is not wise for customers to believe statements/claims about the alleged benefits of products, services, persons who perform services unless the complete name of the source(s) and complete address(s) of the source(s) of said statements/claims is visible in the same location where said statements/claims were published. Based on information from said newspaper, all contents in said newspaper and magazine is copyrighted. So, apparently, customer victims who believed recommendations for products, services, persons who perform services cannot use as evidence, portions of said newspaper wherein said recommendations were published. Similarly, apparently, customers who believed alleged benefits of products, services, persons who render services, which were published in said newspaper or magazine, cannot use as evidence, the portion(s) of the newspaper or magazine wherein said recommendations were published.
warning to people who use Norton Internet Security Suite 2008 computer program. I saw a warning, for said users,at the website of Symantec.
Falls and Older Adults
http://nihseniorhealth.gov/falls/toc.html
About Falls
Many people have a friend or relative who has fallen. The person may have slipped while walking or felt dizzy and fallen when standing up from a chair. Maybe you've fallen yourself.
If you or an older person you know has fallen, you're not alone. The risk of falling -- and fall-related problems -- rises with age.
Among older adults(in America), falls are the number one cause of fractures, hospital admissions for trauma, loss of independence, and injury deaths.
Fractures caused by falls can lead to hospital stays and disability. Most often, fall-related fractures are in the person's hip, pelvis, spine, arm, hand, or ankle.
Hip fractures are one of the most serious types of fall injury. They are a leading cause of medical problems and death among older adults (in America). (In America) only half of older adults hospitalized for a broken hip can return home or live on their own after the injury. Osteoporosis, a disease that involves loss of bone mass, increases the chance of hip and other fractures if a person falls.
Many older adults are afraid of falling. This fear becomes more common as people age, even among those who haven't fallen. It may lead older people to avoid activities such as walking, shopping, or taking part in social activities.
If you're worried about falling, talk with your doctor or another health care provider. Your doctor might refer you to a physical therapist, or PT. A PT can help you improve your balance and walking and help build your walking confidence.
Getting rid of your fear of falling can help you to stay active, maintain your physical health, and prevent future falls.
If you fall, be sure to discuss the fall with your doctor, even if you aren't hurt. Many underlying causes of falls can be treated or corrected. For example, falls can be a sign of a problem with your medicines that can be corrected. They can also be a sign of a manageable disease or other problem, such as diabetes or low blood pressure when you stand.
After a fall, your doctor may suggest physical therapy, use of a walking aid, or other steps to help prevent future falls.
These steps can also make you more confident in your abilities.
Exercise to improve your balance and strengthen your muscles helps to prevent falls. Changing your medicines or your eyewear prescription can help, too. You can also make your home safer to avoid falling.
Falls are not an inevitable part of life, even as a person gets older. You can take action to prevent falls. Your doctor or other health care providers can help you decide what changes will help.
Causes and Risk Factors
Falls don't "just happen," and people don't fall because they get older. Often, more than one underlying cause or risk factor is involved in a fall. A risk factor is something that increases a person's risk or susceptibility to a medical problem or disease.
As the number of risk factors rises, so does the risk of falling. Many falls are linked to a person's physical condition or a medical problem, such as a chronic disease. Other causes could be safety hazards in the person's home or community
environment.
Scientists have linked a number of personal risk factors to falling. Muscle weakness, especially in the legs, is one of the most important risk factors. Older people with weak muscles are more likely to fall than are those who maintain their muscle
strength, as well as their flexibility and endurance.
Older Adults and Balance Problems
Your balance and your gait -- how you walk -- are other key factors. Older adults who have poor balance or difficulty walking are more likely than others to fall. These problems may be linked to a lack of exercise or to a neurological cause,
arthritis, or another condition that might be treated or managed.
Blood pressure that drops too much when you get up from lying down or sitting can increase your chance of falling. This condition -- called postural hypotension -- might result from a drop in blood volume, dehydration, or certain medications.
It might also be linked to diabetes, Parkinson's disease, or an infection.
Some people with postural hypotension feel dizzy when their blood pressure drops. Other people don't feel dizzy, even if their blood pressure drops a lot when they get up.
Your reflexes may also be slower than when you were younger. The increased amount of time it takes you to react may make it harder to catch your balance if you start to fall.
Foot problems that cause painful feet, and wearing unsafe footwear can increase your chance of falling. Backless shoes and slippers, high-heeled shoes, and shoes with smooth leather soles are examples of unsafe footwear that could cause a fall.
Sensory problems can cause falls, too. If your senses don't work well, you might be less aware of your environment. For instance, having numb feet may mean you don't sense where you are stepping.
Not seeing well can also result in falls. One reason is that it may take a while for your eyes to adjust to see clearly when you move between darkness and light.
Other vision problems include poor depth perception, cataracts, and glaucoma. Wearing multi-focal glasses while walking or having poor lighting around your home can also lead to falls.
Confusion, even for a short while, can sometimes lead to falls. For example, if you wake up in an unfamiliar environment, you might feel unsure of where you are. If you feel confused, wait for your mind to clear or until someone comes before trying to get up and walk around.
Medication use can increase a person's risk of falling, too. Sometimes the increased risk is because of the health problems for which the person takes the medications. In other cases, medications cause side effects like dizziness or confusion. Drug interactions can also lead to falls.
The more medications you take the more likely you are to fall. People who take four or more prescription drugs have a greater risk of falling than do people who take fewer drugs.
Never add or stop taking medications without talking with your doctor first. Also, ask your doctor if changes in your medications could lower your risk of falls. Your doctor can tell you which drugs, including over-the-counter medicines, might cause problems.
Be sure to talk with your doctor if you fall, as well. A fall could be a sign of a medical problem such as an infection or a cardiovascular disorder. It could also suggest that a chronic ailment, such as Parkinson's disease or dementia, is
progressing.
Although falls can happen anywhere, well over half of all falls (in America) happen at home. Falls at home (in America) often happen while a person is doing normal daily activities. Some of these falls are caused by factors in the person's living environment. For instance, a slick floor or a poorly lit stairway may lead to a fall.
Other factors that can lead to falls at home include loose rugs, clutter on the floor or stairs, and carrying heavy or bulky things up or down stairs. Not having stair railings and not having grab bars in the bathroom can also result in falls.
Simple changes can help make your home safer. The section called Preventing Falls and Fractures -- Home Safety offers some tips for preventing falls at home.
Falls can happen anywhere, but more than half of all falls happen at home. They often happen while a person is doing normal daily activities.
Some factors in people's living environments that can lead to falls are slick floors, poorly lit stairways, loose rugs, and clutter on floors or stairs. Not having stair railings and not having grab bars in the bathroom can also result in falls.
Simple changes can make your home safer.
Preventing Falls and Fractures
Falls and fractures are not an inevitable part of growing older. Many can be prevented. To reduce your risk of falls and
fractures, you can
* make personal changes that involve your lifestyle or physical well-being
* make changes in your home
* consider using walking aids or other assistive devices
* take steps to maintain or improve your bone health.
Talk with your doctor or another health care professional about how to prevent falls at home and elsewhere.
Preventing Falls and Fractures - Personal Changes
Many falls result from personal or lifestyle factors that can be changed. Your doctor or other health care provider can assess your risk of falling and suggest ways to prevent falls.
At your next check-up, talk with your health care provider about your risk of falling and changes you might make. You might be referred to another health care provider who can help. Also, let your doctor know if you've fallen or almost fallen.
Here are some changes you might make.
* Be physically active.
* Have your medicines reviewed.
* Have your blood pressure checked when lying and standing.
* Get a vision check-up.
* Choose safe footwear.
Why Older Adults Should Exercise
Be Physically Active
Regular physical activity is a first line of defense against falls and fractures. Physical activity strengthens muscles and increases flexibility and endurance. In turn, your balance and the way you walk may change, decreasing the chances of a
fall.
It's important to keep muscles strong. Strengthening muscles in the lower body can improve balance. Work with your doctor or a physical therapist to plan a physical activity program that is right for you.
A supervised group program can help with balance and gait training. Strength and balance exercises done at home can also reduce your risk of falls. Whether done with a group or on your own, be sure your program becomes more challenging over
time. This will help improve your balance and strength.
Tai Chi is one type of exercise that may help prevent falls by improving balance and control. This exercise uses slow, flowing movements to help people relax and coordinate the mind and body. It can also boost your self-confidence. Dancing
and other rhythmic movements can help as well.
Doing Strength Exercises
Mild weight-bearing exercise -- such as walking or climbing stairs -- may help slow bone loss from osteoporosis. Having strong bones can prevent fractures if you do fall.
Your doctor or a physical therapist can check your walking and balance. They might do a "Get-Up and Go" test. This simple test shows how steady you are when you get up from a chair. The test also is used to check your walking ability.
Have Your Medicines Reviewed
Find out about the possible side effects of medicines you take. Some medications might affect your coordination or balance, or cause dizziness, confusion, or sleepiness. Some medications don't work well together, adding to your risk of falls.
Bring your prescribed and over-the-counter medicines with you when you visit the doctor. Also bring any vitamins, minerals, and herbal products you are taking.
Ask if any of your medicines or over-the counter products could increase your risk of falling. Also ask if you no longer need to take any of your medications or if the doses might be decreased. Never stop taking your medications unless you talk
with your doctor first.
Also, limit the amount of alcohol you drink. Even a small amount can affect your balance and reflexes.
Have Your Blood Pressure Checked When Lying and Standing
Some older people have normal or increased blood pressure while seated, but their blood pressure drops too much on standing. There is no way to know unless you check. Most often, though, your blood pressure is checked when you are
sitting.
Your health care provider should check your blood pressure and pulse after you have been lying down for at least 5 minutes and again after you get up. If it drops too much when you get up, ask if any of your medications may be decreased or if you
should make other changes. Drinking more water, getting up more slowly, pumping your feet or hands before getting up, or wearing special stockings can help, too.
Get a Vision Check-Up
Have your vision tested regularly or if you think it has changed. Even small changes in sight can make you less stable.
Wear your eyeglasses so you can see your surroundings clearly. Keep them clean and check to see that the frames are straight.When you get new glasses, be extra cautious while you are getting used to them. If you use reading glasses or multi-focal
lenses, take them off when you're walking.
Choose Safe Footwear
The soles of our feet have nerves that help us judge the position of our bodies. To work correctly, our feet need to be in touch with the ground and our shoes need to stay securely with the foot as we take each step. Otherwise, falls may occur.
Characteristics of a good shoe.
It's important to select your footwear carefully to help prevent falls. Wear sensible, low-heeled shoes that fit well and support your feet. There should be no marks on your feet when you take off your shoes and socks.Your shoes should completely surround your feet. Wearing only socks or wearing floppy, backless slippers or shoes without backs can be unsafe. Also, choose shoes with non-slip soles. Smooth soles can cause you to slip on waxed or polished floors.
Preventing Falls and Fractures - Home Safety
(In America) six out of every 10 falls happen at home, where we spend much of our time and tend to move around without thinking about our safety. Many falls could be prevented by making simple changes in your living areas, as well as personal
and lifestyle changes.
Take steps to "fall proof" your home, both inside and outdoors. To make your home safer, you can
* remove or avoid safety hazards
* improve lighting
* install handrails and grab bars
* move items to make them easier to reach.
An important step toward preventing falls at home is to remove anything that could cause you to trip or slip while walking. Tripping on clutter, small furniture, pet bowls, electrical or phone cords, or other things can cause you to fall. Slipping
on rugs or slick floors can also cause falls.Arrange furniture to give you plenty of room to walk freely. Also remove items from stairs, hallways, and pathways.Be sure that carpets are secured to the floor and stairs. Remove throw rugs, use non-slip rugs, or attach rugs to the floor with double-sided tape.Put non-slip strips on floors and steps. Put non-slip strips or a rubber mat on the floor of your bathtub or shower, as well. You can buy these items at a home center or hardware store.
At home and elsewhere, try to avoid wet floors and clean up spills right away. Use only non-skid wax on waxed floors at home. Be careful when walking outdoors, and avoid going out on ice or snow. A simple slip on a slick sidewalk, a curb, or icy
stairs could result in a serious injury.
A cane or walker might make you more stable in bad weather. During the winter, ask someone to spread sand or salt on icy surfaces. Be sure to wear boots with good traction if you must go out when it snows. Better yet, don't take chances walking
on icy or slippery surfaces.
Poor lighting -- inside and outdoors -- can increase your risk of falls. Make sure you have enough lighting in each room, at entrances, and on outdoor walkways. Use light bulbs that have the highest wattage recommended for the fixture. Good lighting on stairways is especially important. Light switches at both the top and bottom of stairs can help.Place a lamp within easy reach of your bed. Put night lights in the bathroom, hallways, bedroom, and kitchen. Also keep a flashlight by your bed in case the power is out and you need to get up.
Have handrails installed on both sides of stairs and walkways. If you must carry something while walking up or down stairs, hold the item in one hand and use the handrail with the other. When you're carrying something, be sure you can see where
your feet are stepping.Properly placed grab bars in your tub and shower, and next to the toilet, can help you avoid falls, too. Have grab bars installed, and use them every time you get in and out of the tub or shower. Be sure the grab bars are securely attached to the wall.
You might find it helpful to rearrange often-used items in your home to make them more accessible. Store food boxes, cans, dishes, clothing, and other everyday items within easy reach. This simple change could prevent a fall that might come from
standing on a stool to get to an item.
If you have fallen, your doctor might suggest that an occupational therapist, physical therapist, or nurse visit your home. These health care providers can assess your home's safety and advise you about making changes to prevent falls.
Preventing Falls and Fractures - Helpful Devices
Use of assistive devices can prevent harmful falls. These devices include canes, walkers, and reachers. A physical or occupational therapist can help you decide which devices might be helpful and how to use them safely. Talk with your doctor about having a physical therapist assess your device needs.
A cane or walker can help you feel more stable when you walk. Walking aids are especially helpful when you're in places you don't know or where walkways are uneven.
Different types of canes are available. Some have grips made of foam or that fit the shape of your hand. Many canes can be adjusted, but some cannot.
A physical therapist can advise you about which cane to choose. Be sure the length fits you well. Your elbow should be at a comfortable angle. A cane that's too short may make you unsteady. A cane that's too long is harder to use. If you use a
cane, be sure to learn how to walk with it the right way. A physical therapist can help.
If you're at risk of falling, your doctor or physical therapist might suggest using a walker. A walker will help you stay balanced by giving you a wide base of support. Be sure to choose a walker that fits you and gives a level of stability that is best for you.
Different types of walkers are available. Some walkers have two wheels so the walker shouldn't roll away from you. These walkers work well if you need to put weight on the walker when you move. Other walkers have four wheels and brakes for going down inclines.
You can add a basket, tray, or pouch to some walkers to carry items. These ccessories will make it more convenient to use the walker.
If you use a walker, be sure it's the right type for you. Also, use it when needed and use it properly. A health care professional can help you select the right walker and show you how to use it.
A reacher, or grabber, can also help prevent falls. This simple tool lets you take lightweight items from high shelves and other places. Use a reacher rather than standing on a stool to get something from above.
Another helpful device is a portable telephone. Carry the phone with you from room to room. When it rings, you won't have to rush to answer it. Not rushing could avert a harmful fall.
Preventing Falls and Fractures - Bone Health
Falls are a common reason for trips to the emergency room and for hospital stays among older adults. Many of these hospital visits are for fall-related fractures. You can help prevent fractures by maintaining the strength of your bones.
Having healthy bones won't prevent a fall. If you fall, though, having healthy bones can prevent hip or other fractures that may lead to a hospital or nursing home stay, disability, or even death.
Osteoporosis makes bones thin and more likely to break. It is a major reason for fractures in women past menopause. It also affects older men. If bones are fragile, even a minor fall can cause fractures.
At any age, you can take steps to keep your bones strong. Be sure to consume adequate amounts of calcium and vitamin D. People over age 50 should consume 1,200 mg of calcium daily by eating calcium-rich foods and taking calcium supplements.
Good dietary sources of calcium include
* dairy products such as low-fat milk, yogurt, and cheese
* orange juice, cereals, and other foods fortified with calcium
* dark green, leafy vegetables such as broccoli, collard greens, and bok choy
* sardines, salmon with bones, soybeans, tofu, and nuts such as almonds.
Vitamin D helps your body absorb calcium. Exposure to sunlight causes your body to make vitamin D. Many older people don't get enough vitamin D this way, though. Eating foods with vitamin D and taking supplements can help. As you grow older, your need for vitamin D increases. People ages 51 to 70 should consume at least 400
international units (IU) of vitamin D daily. People over age 70 should consume at least 600 IU daily.
Herring, sardines, salmon, tuna, liver, eggs, and fortified milk and foods are good sources of vitamin D. Vitamin D supplements may also be needed. Talk with your doctor about how much vitamin D you need. Taking too much may be harmful.
Physical activity is another way to keep your bones strong. Try to get a total of at least 30 minutes of physical activity a day. Find time for activities like walking, dancing, stair climbing, gardening, and weight-lifting.
Talk with your doctor about having a bone density test. This safe, painless test assesses your bone health and risk of future fractures. (In America) Medicare and many private insurers cover this test for eligible people. Women over age 65
and all men over 70 should have a bone density test.
Your doctor can also advise you about whether you should consider taking prescription medications to improve bone health. These medications can slow bone loss, improve bone density, and lessen the risk of fractures.
Other ways to maintain bone health include quitting smoking and limiting alcohol use. Smoking and heavy alcohol use can decrease bone mass and increase the chance of fractures. Also, maintain a healthy weight. Being underweight increases the
risk of bone loss and broken bones.
You're never too old to improve your bone health. A diet that includes enough calcium and vitamin D, and physical activity can help prevent bone loss and fractures. You can also have your bone density tested and ask your doctor about supplements or other medicines to strengthen your bones if needed.
If You Fall
Whether you're at home or somewhere else, a sudden fall can be startling and upsetting. If you do fall, stay as calm as possible. Take several deep breaths to try to relax.
Remain still on the floor or ground for a few moments. This will help you get over the shock of falling. It will also give you time to decide if you're hurt before getting up. Getting up too quickly or in the wrong way could make an injury worse.
If you think you can get up safely without help, roll over onto your side. Push yourself up into a seated position. Rest again while your body and blood pressure adjust. Slowly get up on your hands and knees, and crawl to a sturdy chair.Put your hands on the chair seat and slide one foot forward so that it is flat on the floor. Keep the other leg bent so the knee is on the floor. From this kneeling position, slowly rise and turn your body to sit in the chair.If you're hurt or can't get up on your own, ask someone for help or call (the emergency number). If you're alone, try to get into a comfortable position and wait for help to arrive.
If you have problems with balance or dizziness and are often alone, consider getting a personal emergency response system. This service, which works through your telephone line, provides a button or bracelet to wear at all times in your home.
If you fall or need emergency assistance for any reason, a push of the button will alert the service. Emergency medical services will be called. There is a fee for medical monitoring services, but your personal safety may be worth the cost.
Carrying a portable phone with you as you move about your house could make it easier to call someone if you need assistance. You might also put a telephone in a place that you can reach from the floor in case you fall and need help.
Be sure to discuss any fall with your doctor. Write down when, where, and how you fell so you can discuss the details with your doctor. The doctor can assess whether a medical issue or other cause of the fall needs to be addressed. Knowing the
cause can help you plan to prevent future falls.
Many older people who have fallen are afraid of falling again. Even if a fall doesn't cause injury, the fear of falling again might prevent you from doing activities you enjoy or need to do. Fear of falling also might cause you to stay at home away from your friends, family, and others.
Your muscles and bones can weaken over time without the physical activity that comes with doing daily tasks or exercise. As a result, you could become more -- not less -- likely to fall.
After a fall, your doctor might refer you to other health care providers who can help prevent future falls. A physical therapist can help with gait, balance, strength training, and walking aids. An occupational therapist can suggest changes in your home that may lower your risk of falls.
If you're at high risk for falls and hip fractures, your doctor might suggest that you wear a padded "hip protector." A hip protector is worn over the hips under clothing. It absorbs some of the force of a fall and lessens the impact of the fall
on the bones.
Frequently Asked Questions
1. How common are falls among older people?
(In America) more than one in three people age 65 years or older fall each year. The risk of falling -- and the risk of disability and other life-changing problems caused by falls -- increase with age. Falls are not an inevitable part of getting older, though. Many falls can be prevented.
2. Why do people fall?
People fall for many reasons. Often, more than one risk factor is involved in a fall. As the number of risk factors rises, so does the risk of falling.
Many falls are linked to personal factors -- a person's physical condition or medical problems. Falls may also be linked to safety hazards in the person's home or community environment.
3. What personal factors can lead to falls?
Older Adults and Balance ProblemsSome personal factors that can lead to falls are
* muscle weakness, especially in the legs
* poor balance or difficulty walking -- factors that could be related to a
neurological cause, arthritis, or another condition that might be treated.
* blood pressure that drops too much on standing
* vision problems
* taking medications that cause side effects like dizziness and confusion, or
that interact with one another.
Impaired mental abilities and urinary incontinence may also contribute to falls.
4. What environmental factors can lead to falls?
Some environmental factors that can lead to falls are
* clutter and other tripping hazards
* slick floors, loose rugs, and slippery walkways
* poor lighting, either inside or outdoors
* not having handrails along stairs and grab bars in the bathroom.
5. How do falls affect people?
Falls most often result in bruises or minor cuts, but they sometimes affect a erson's physical or mental well-being. At least one-tenth of falls result in serious injury to soft tissues or bones. A fall can cause a fracture, head injury, or other problem that can change a person's life.
Fractures caused by falls can lead to hospital stays and disability. They can also prevent a person from getting around, doing daily tasks, or socializing. Most often, fall-related fractures are in the person's hip, pelvis, spine, arm, hand, or
ankle.
Fear of falling again can cause problems. A person who has fallen may avoid doing daily tasks or enjoyable activities. This fear can also cause the person to spend more time at home, away from other people.
6. How common are hip fractures, and what problems do they cause?
(In America) hip fractures are a common and very serious type of fall-related injury among older adults. These fractures are a leading cause of medical problems, loss of independence, and death. Only half of older adults hospitalized for a broken hip will be able to get around as they did before the hip fracture. Many will need long-term care.
7. What is osteoporosis and who gets it?
Oteoporosis is a disease that involves loss of bone mass. Over time, this disease thins and weakens bones to the point where they break easily, especially in the hip, spine, and wrist. Low bone mass increases the chance of hip fractures and
other fractures if you fall. If bones are fragile, even a minor fall can cause fractures.
More than two-thirds of people with osteoporosis are women, but men can also have it. Small, thin-boned women and women who are Caucasian or Asian are at greatest risk.
8. How do I know if I have osteoporosis?
Osteoporosis has no symptoms. Many people don't know they have it until a bone breaks. A bone density test can tell you if you are at risk. This safe, painless test uses X-rays or sound waves to measure the strength of your bones. Women over age
65 and men over 70 should have a bone density test.
9. How can I improve my bone health?
Getting enough calcium and vitamin D, and staying physically active can help keep bones healthy and prevent bone loss. Not smoking and limiting the amount of alcohol you drink can help, too. Your doctor might also recommend taking medicines to slow bone loss or help rebuild bone if you are at risk of osteoporosis.
10. How much calcium and vitamin D do I need to keep my bones strong?
Vitamin D chart.People over age 50 should consume 1,200 mg of calcium daily by eating calcium-rich foods and taking calcium supplements. People ages 51 to 70 should consume at least 400 international units (IU) of vitamin D daily. People over age
70 should consume at least 600 IU daily.
11. Can medications increase my risk of falling?
People who take at least four prescription drugs have a greater risk of falling than do people who take fewer drugs. Sometimes the increased risk comes from the health problems for which the person takes the medications. In other cases, the effects of the medications themselves increase a person's risk of falls.
Certain medications cause side effects like dizziness, confusion, and sleepiness that increase a person's risk of falling. Some medications don't work well together and may cause problems that lead to falls.
If you think your medicines are causing problems, don't stop taking them unless you talk with your doctor first. Also, be sure to talk with your doctor about your risk of falls from medications.
12. Should I talk with my doctor about changing my medications to help prevent falls?
It is important to talk with your doctor about your medications. Bring your prescribed medicines with you when you visit the doctor. Also bring any over-the-counter products, vitamins, minerals, and herbal products you are taking.
Ask if any of the medications or other products might increase your risk of falling. Also ask if you no longer need to take any of the medicines or if the doses might be decreased.
13. Does physical activity increase my risk of falls?
Why Older Adults Should Exercise
You might think that moving about will increase the chance of falling. However, physical activity actually helps lower older adults' risk of falls.
Why Exercise
Without the physical activity that comes with doing daily tasks or exercise, your muscles and bones can weaken over time. As a result, you could become more -- not less -- likely to fall. Talk with your doctor about what kinds of physical activity you should do.
14. How does exercise help prevent falls?
Getting regular exercise is one way to prevent falls and fractures that result from falls. Exercise keeps muscles strong and improves balance. It also helps keep joints, tendons, and ligaments flexible. In turn, your balance and the way you walk may improve, lowering your risk of falling.
Your doctor or a physical therapist can help you plan an exercise program that is right for you. A supervised group program can improve your balance and gait. Doing strength and balance exercises at home can also reduce your risk of falls.
15. Does physical activity help prevent fractures?
Regular physical activity helps slow bone loss and builds strong bones. Having strong bones can prevent fractures if you do fall. Walking, dancing, climbing stairs, gardening, and doing other physical activities at least 30 minutes a day can help
keep bones healthy.
16. What is Tai Chi and how can it help prevent falls?
Tai Chi is an ancient Chinese method of using slow, flowing movements to coordinate the mind and body. This gentle, relaxing activity can improve strength, balance, postural alignment, and concentration.
Some studies have found that Tai Chi helps prevent falls among older people because it improves balance and control. It may also boost self-confidence and reduce the fear of falling.
17. Where can I learn more about exercise and older adults?
NIHSeniorHealth.gov includes a section about exercise and older adults.
The National Institute on Aging also offers Exercise: A Guide from the National Institute on Aging and a companion video, available in both English and Spanish.
18. Can vision problems lead to falls?
Vision problems can contribute to falls among older people. Problems that can lead to falls include
* lack of depth perception or visual sharpness
* not being able to see contrasting objects
* cataracts
* glaucoma.
19. What can I do to prevent vision-related falls?
Photo of a woman and her eye doctor.Have your vision tested regularly or if you think it has changed. Even a small change in vision can increase your risk of falling.
To prevent falls, wear your eyeglasses if you need them. Keep the lenses clean and be sure the frames are straight. If you get new glasses, be extra cautious as you get used to them. If you wear reading glasses or multi-focal lenses, take them
off when you're walking to avoid missteps.
20. What kind of footwear should I wear to help prevent falls?
Sensible footwear can help prevent falls. Choose shoes that
* have low heels and non-slip soles
* fit well -- there should be no marks on your feet when you take off your
shoes and socks
* completely surround the foot -- no backless shoes
* support your feet.
Characteristics of a good shoe.Avoid wearing only socks or floppy, backless slippers. Also, be sure to wear boots with good traction if you go outside in the snow.
21. Where do most falls happen?
Falls can happen anywhere, but more than half of all falls happen at home. Many of these falls could be prevented by making simple changes in the home.
22. What can I do to prevent falls at home?
One simple way to prevent falls at home is to remove objects from stairs, hallways, and other places where you walk. Tripping on clutter, shoes, small furniture, pet bowls, electrical or phone cords, or other things can cause a fall. Be sure to arrange furniture so you have plenty of room to walk freely, too.
Secure carpets to the floor and stairs. Remove throw rugs, use non-slip rugs, or attach rugs to the floor with double-sided tape. Put non-slip strips on floors and steps. Put non-slip strips or a rubber mat on the floor of your bathtub or shower.
Have handrails installed along stairs. Have grab bars installed in the tub and shower and next to the toilet. Be sure the handrails and grab bars are firmly attached to the wall.
Re-arranging items in your home can also help prevent falls. Place often-used items within easy reach so you don't need to stand on a stool to get them.
23. Can better lighting help prevent falls?
Good lighting can help prevent falls. Make sure you have adequate lighting in each room, at entrances to your home, and on stairways in your home. Light switches at both the top and bottom of stairs can help. Throughout your home, use light bulbs
that have the highest wattage recommended for the fixture.
Place night lights in the bathroom, hallways, and other areas to guide you when you get up at night. You might also put a lamp within reach of your bed. Keeping a flashlight near your bed can help if the power is out and you need to get up.
24. What can I do to prevent falls outdoors?
Be careful when walking outdoors. Slipping on a slick sidewalk, a curb, or icy stairs could result in a disabling fracture or other injury.
To help prevent falls outdoors at home, you should
* have handrails installed on both sides of outdoor stairs and walkways
* use a cane or walker to increase your stability and walking confidence in bad
weather
* light stairs and walkways
* ask someone to spread sand or salt on icy surfaces
* wear shoes or snow boots with traction when walking on slippery surfaces.
25. Should I use a cane to avoid falls?
Talk with your doctor or a physical therapist to find out if a walking aid will help you avoid falls. A cane or walker could make you more stable when you walk. This walking aid might be especially helpful when you're in unfamiliar places or
where walkways are uneven.
26. If I need a cane, what size should I have?
Be sure that your cane fits you well and that you learn to use it safely. The height of a cane should allow your elbow to be at a comfortable angle. A physical therapist can help you choose the right size and type of cane and can show you how to use it properly.
27. Should I use a walker to prevent falls?
Ask your doctor if a walker would help you prevent falls. A walker could help you stay balanced by giving you a wide base of support. Take time to learn how to use a walker properly. Also, be sure to use the walker when needed.
28. How can I choose the right kind of walker if I need one?
If you need to use a walker, it is important to choose the right kind for you. It's also important to develop a habit of using any walking aid correctly. A physical therapist can help you choose a walker that meets your needs and fits you well.
Two-wheeled walkers won't roll away when you put weight on the walker. Four-wheeled walkers can be used if you don't need to put your weight on the walker for balance.
When using a walker, your elbows should be at a comfortable angle of about 30 degrees. Also, when your arms are relaxed at your sides, the inside of your wrist should be at the top of the walker grip.
29. What should I do if I fall?
A sudden fall can be startling and frightening. If you fall, try to stay calm. Take a few deep breaths to help you relax.Stay still on the floor or ground for a few moments to help you get over the shock of falling. It will also give you time
to decide if you're hurt before getting up. Getting up too quickly or in the wrong way could make an injury worse.
How to get up from a fall.If you think you can get up safely without help, you should follow these steps.
* Roll over onto your side and push yourself up into a seated position.
* Rest while your body and blood pressure adjust.
* Slowly get up on your hands and knees, and crawl to a sturdy chair.
* Put your hands on the chair seat and slide one foot forward so that it is
flat on the floor. Keep the other leg bent
so the knee is on the floor.
* From this kneeling position, slowly rise and turn your body to sit in the
chair.
If you're hurt or can't get up, ask someone for help or call 911. If you're alone, try to get into a comfortable position and wait for help to arrive.
30. Should I tell my doctor if I fall?
Yes. Be sure to tell your doctor if you fall or almost fall, even if you aren't hurt. The fall might be a sign of an underlying problem that can be treated or corrected.
Write down when, where, and how you fell so you can discuss the details with your doctor. The doctor can assess whether a medical issue, such as low blood pressure or diabetes, or another cause of the fall should be addressed.
Knowing the cause of a fall can help you and your doctor find ways to prevent future falls. For instance, your doctor might suggest changing your medication doses or eyewear prescription.
31. How can I cope with my fear of falling?
Many older adults are afraid of falling. This fear becomes more common as people age, even among those who haven't fallen. Getting rid of your fear of falling can help you to stay active, maintain your physical health, and prevent future falls.
Fear of falling might cause you to avoid doing activities you enjoy or need to do. It might also cause you to stay at home, away from your friends, family, and others. In turn, you may become lonely and inactive.
If you're worried about falling, talk with your doctor. He or she may be able to help you cope with this concern by referring you to a physical therapist. A physical therapist can help you improve your balance and help build your walking
confidence.
32. Why do I sometimes feel dizzy when I stand up?
Dizziness might be caused by postural hypotension -- a drop in blood pressure when you stand up. This condition might result from a drop in blood volume, dehydration, or certain medications. It might also be linked to diabetes, Parkinson's disease, or an infection.
Why Am I Dizzy?Talk with your doctor if you sometimes feel dizzy when you stand up. The doctor or a nurse can check your blood pressure to find out if you have postural hypotension. Some people with postural hypotension do not feel dizzy so it is important to ask your doctor or nurse to check your blood pressure while you are lying and standing. They can also suggest ways to avoid the dizziness that could result in a fall. For instance, the doctor may suggest drinking more water
or changing some of your medicine doses. There may also be other reasons for your dizziness which your doctor can help you identify.
Also, always stand up slowly after eating, lying down, or resting. Getting up too quickly can cause your blood pressure to drop.
33. Should I get a personal emergency response system?
If you have problems with balance or dizziness or live alone, you might want to get a personal emergency response system. This service provides a button or bracelet to wear at all times in your home.
If you fall or need emergency medical assistance for any reason, a push of the button will alert the service through the phone system. Emergency medical services will be called. There is a fee for medical monitoring services, but it may be worth the cost.
34. Where can I learn more about preventing falls?
MedlinePlus, a service of the National Library of Medicine, provides more resources about falls and fall prevention.
http://www.nlm.nih.gov/medlineplus/falls.html
Topic last reviewed: 16 October 2006
Topic first published: 16 October 2006
web sites with free useful information:
cookinglight web site
http://www.cookinglight.com/cooking/0,14319,,00.html
Subscribe to:
Post Comments (Atom)
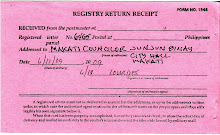
image of registry return receipt of letter addressed to Makati councilor J. J. Binay

No comments:
Post a Comment