USDA CONSUMER ALERT: Keeping Food Safe During An Emergency
http://www.fsis.usda.gov/News_&_Events/NR_031810_01/index.asp
WASHINGTON - March 18, 2010 -
Steps to follow to prepare for a possible weather emergency:
* Keep an appliance thermometer in the refrigerator and freezer. An appliance thermometer will indicate the temperature inside the refrigerator and freezer in case of a power outage and help determine the safety of the food.
* Make sure the freezer is at 0° F or below and the refrigerator is at 40° F or below.
* Freeze containers of water for ice to help keep food cold in the freezer, refrigerator or coolers after the power is out.
* Freeze refrigerated items such as leftovers, milk and fresh meat and poultry that you may not need immediately — this helps keep them at a safe temperature longer.
* Plan ahead and know where dry ice and block ice can be purchased.
* Have coolers on hand to keep refrigerator food cold if the power will be out for more than 4 hours. Purchase or make ice cubes and store in the freezer for use in the refrigerator or in a cooler. Freeze gel packs ahead of time for use in coolers.
* Group food together in the freezer — this helps the food stay cold longer.
* Store food on shelves that will be safely out of the way of contaminated water in case of flooding.
Steps to follow after the weather emergency:
* Keep the refrigerator and freezer doors closed as much as possible to maintain the cold temperature.
* The refrigerator will keep food safely cold for about 4 hours if it is unopened. A full freezer will hold the temperature for approximately 48 hours (24 hours if it is half full) and the door remains closed.
* Discard refrigerated perishable food such as meat, poultry, fish, soft cheeses, milk, eggs, leftovers and deli items after 4 hours without power.
* Food may be safely refrozen if it still contains ice crystals or is at 40° F or below when checked with a food thermometer.
* Never taste a food to determine its safety!
* Obtain dry or block ice to keep your refrigerator and freezer as cold as possible if the power is going to be out for a prolonged period of time. Fifty pounds of dry ice should hold an 18-cubic-foot full freezer for 2 days.
* If the power has been out for several days, check the temperature of the freezer with an appliance thermometer. If the appliance thermometer reads 40° F or below, the food is safe to refreeze.
* If a thermometer has not been kept in the freezer, check each package of food to determine its safety. If the food still contains ice crystals, the food is safe.
* Discard any food that is not in a waterproof container if there is any chance that it has come into contact with flood water. Discard wooden cutting boards, plastic utensils, baby bottle nipples and pacifiers.
* Thoroughly wash all metal pans, ceramic dishes and utensils that came in contact with flood water with hot soapy water and sanitize by boiling them in clean water or by immersing them for 15 minutes in a solution of 1 tablespoon of unscented, liquid chlorine bleach per gallon of drinking water.
* Undamaged, commercially prepared foods in all-metal cans and retort pouches (for example, flexible, shelf-stable juice or seafood pouches) can be saved. Follow the Steps to Salvage All-Metal Cans and Retort Pouches in the publication "Keeping Food Safe During an Emergency" at: www.fsis.usda.gov/Fact_Sheets/
Keeping_Food_Safe_During_an_Emergency/index.asp
* Use bottled water that has not been exposed to flood waters. If bottled water is not available, tap water can be boiled for safety. For more information on drinking water safely during weather emergencies, access the FSIS publication "Keeping Food Safe During an Emergency" at: www.fsis.usda.gov/Fact_Sheets/
Keeping_Food_Safe_During_an_Emergency/index.asp
* When in Doubt, Throw it Out!
Tips to Prevent Poisonings
http://www.cdc.gov/HomeandRecreationalSafety/Poisoning/preventiontips.htm
Safety Tips for You, Your Family, and Friends
Unless noted, the safety tips below were adapted from the American Association of Poison Control Centers’ poison prevention tips for children and adults.
Drugs and Medicines
* Follow directions on the label when you give or take medicines. Read all warning labels. Some medicines cannot be taken safely when you take other medicines or drink alcohol.
* Turn on a light when you give or take medicines at night so that you know you have the correct amount of the right medicine.
* Keep medicines in their original bottles or containers.
* Never share or sell your prescription drugs.
* Keep opioid pain medications, such as methadone, hydrocodone, and oxycodone, in a safe place that can only be reached by people who take or give them.
* Monitor the use of medicines prescribed for children and teenagers, such as medicines for attention deficit disorder, or ADD (SAMHSA 2006).
* Dispose of unused, unneeded, or expired prescription drugs. Follow the federal guidelines for how to do this (ONDCP 2009).External Web Site Icon
Household Chemicals and Carbon Monoxide
* Always read the label before using a product that may be poisonous.
* Keep chemical products in their original bottles or containers. Do not use food containers such as cups, bottles, or jars to store chemical products such as cleaning solutions or beauty products.
* Never mix household products together. For example, mixing bleach and ammonia can result in toxic gases.
* Wear protective clothing (gloves, long sleeves, long pants, socks, shoes) if you spray pesticides or other chemicals.
* Turn on the fan and open windows when using chemical products such as household cleaners.
Keep Young Children Safe from Poisoning
* Put the poison control number, on or near every home telephone and save it on your cell phone. The line is open 24 hours a day, 7 days a week.
* Keep all drugs in medicine cabinets or other childproof cabinets that young children cannot reach.
* Avoid taking medicine in front of children because they often copy adults.
* Do not call medicine “candy.”
* Be aware of any legal or illegal drugs that guests may bring into your home. Do not let guests leave drugs where children can find them, for example, in a pillbox, purse, backpack, or coat pocket.
* When you take medicines yourself, do not put your next dose on the counter or table where children can reach them.
* Never leave children alone with household products or drugs. If you are using chemical products or taking medicine and you have to do something else, such as answer the phone, take any young children with you.
* Do not leave household products out after using them. Return the products to a childproof cabinet as soon as you are done with them.
* Identify poisonous plants in your house and yard and place them out of reach of children or remove them.
* Read about how to prevent lead poisoning.
What to do if a poisoning occurs
1. Remain calm.
2. Call 911 if you have a poison emergency and the victim has collapsed or is not breathing. If the victim is awake and alert, dial 1-800-222-1222. Try to have this information ready:
* the victim’s age and weight
* the container or bottle of the poison if available
* the time of the poison exposure
* the address where the poisoning occurred
3. Stay on the phone and follow the instructions from the emergency operator or poison control center.
Poisoning Prevention in Your Community
Raise awareness about unintentional poisonings and to share prevention tips. You can find more information and event materials at the National Poison Prevention Week CouncilExternal Web Site Icon.
You can talk with local schools about teaching poison prevention. Lesson plans are available from the American Association of Poison Control CentersExternal Web Site Icon.
References
Office of National Drug Control Policy. Proper disposal of prescription drugs [online]. [cited 2009 December 2]. Available from URL: http://www.whitehousedrugpolicy.gov/publications/pdf/prescrip_disposal.pdfExternal Web Site Icon
Substance Abuse and Mental Health Services Administration. How do kids get prescription drugs? [online]. [cited 2006 October 26]. Available from URL: http://family.samhsa.gov/monitor/howpresdrug.aspxExternal Web Site Icon
Sources for Additional Information
American Association of Poison Control Centers, Inc.External Web Site Icon
CDC: Carbon Monoxide Poisoning: Prevention Guidelines
Substance Abuse and Mental Health Services AdministrationExternal Web Site Icon
Contact Us:
* Centers for Disease Control and Prevention
National Center for Injury Prevention and Control (NCIPC)
4770 Buford Hwy, NE
MS F-63
Atlanta, GA 30341-3717
* 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348
24 Hours/Every Day
* cdcinfo@cdc.gov
* Page last updated: March 12, 2010
* Content source: Centers for Disease Control and Prevention
* National Center for Injury Prevention and Control
* Links to non-Federal organizations found at this site are provided solely as a service to our users. These links do not constitute an endorsement of these organizations or their programs by CDC or the Federal Government, and none should be inferred. CDC is not responsible for the content of the individual organization Web pages found at these links.
Poison Prevention Tips
http://www.aapcc.org/dnn/PoisoningPrevention/tabid/116/Default.aspx
STORE POISONS SAFELY
* Store medicines and household products locked up, where children cannot see or reach them.
* Store poisons in their original containers.
* Use child-resistant packaging. But remember — nothing is child-proof!
USE POISONS SAFELY
* Read the label. Follow the directions on medicines and products.
* Are children around? Take the product or medicine with you to answer the door or the phone.
* Lock products and medicines up after using them.
* Is it medicine? Call it medicine, not candy.
* Children learn by imitation. Take your medicines where children can’t watch.
TEACH CHILDREN TO ASK FIRST
* Poisons can look like food or drink. Teach children to ask an adult before eating or drinking anything!
Poison Tips for Children
http://www.aapcc.org/dnn/PoisoningPrevention/ChildTips/tabid/120/Default.aspx
* If you don't know what something is, never put it in your mouth. Always ask a trusted grown up first.
* Never take medicine unless a grown-up gives it to you.
* Some plants and berries are poisonous. Always ask a grown-up before you put them in your mouth.
* Always let grown-ups use spray cans and bottles. Do not touch or play with them!
* Stay away from things used to clean your house, clothes or car.
What is a poison?
How can you get poisoned?
You can get poisoned by eating, drinking, touching, or smelling something that can make you sick or hurt you. Some things, like medicine, can make you sick if you take the wrong kind, or if you take too much. Always ask a trusted grown-up before you take any medicine. Never put anything in your mouth if you are not sure if it is safe to eat. Ask a grown-up first!
Where are poisons found?
Poison can be found in any room in your home. They can even be found in Grandma’s purse! Poisons can be found outside, like some plants, berries and mushrooms.
What can you do if someone gets poisoned?
If you think you got into a poison, tell a grown-up right away! They will call the poison center. The poison center will tell them how to help you. If you think your Mom or Dad, or your brother or sister, or even your friend got into a poison, you can call the poison center too. Learn the poison center's phone number: and make sure you have the number of the poison center on or near the telephones in your house.
Poison Tips for Teens
http://www.aapcc.org/dnn/PoisoningPrevention/TeenTips/tabid/121/Default.aspx
Why do babysitters or teens need to know about poison?
Caring for children is a great job, but keeping children safe is a serious and important part of babysitting.
Poisoning is one of the most common childhood injuries.
Most of the time poisoning happens right at home. Children who are between the ages of eight months and six years old are the most likely to be poisoned.
Poisons can look like things that are good to eat and drink. They can come in many colors and forms including solids, liquids, sprays or gases. Young children are curious. They like to put things in their mouth, especially if they look colorful or smell nice. It's a good idea to have emergency information handy when you're babysitting.
What are some common poisons?
Poisonous products that may be found in and around the home:
* medicines
* iron pills
* cleaning products
* cleaning products
* laundry products
* nail glue remover and primer
* batteries
* bug and weed killers
* cigarettes
* alcohol
* mouthwash
* plants (indoor and outdoor)
* lighter fluids
How can children be kept safe from poison?
Follow these safety tips:
* Keep children where you can see them at all times, even when you go to answer the door or telephone. Never leave young children alone, not even for just a minute!
* All medicines and household cleaning products should be stored in locked cabinets, out of the reach and sight of children. Do not leave poisons on a counter or in an unlocked cabinet.
* Never carry something that can be poisonous, such as a medicine, in a purse where children may find it.
* Safety latches on drawers or cabinets, and child resistant caps on bottles, are helpful in keeping poisons out of the hands of children. But remember, they are not “child-proof” and do not substitute for your careful and constant supervision.
Remember the BEFORE, WHILE and AFTER Rule
BEFORE using a cleaning product, read the instructions on the bottle.
WHILE using a cleaning product, never leave it alone. A child may find it.
AFTER using a product, put it back in a locked cabinet. Make sure the container is closed tightly.
If you are asked to give medicine to a child, follow the instructions on the bottle. After using the medicine, return the bottle to a safe storage place right away. Never leave a child alone with the medicine.
What information about each child should you have?
Before parents leave you in charge of a child, make sure they write down some basic information such as:
* each child’s age and weight
* any allergies or medical conditions
* their doctor’s name and telephone number
* how the parents can be reached in an emergency
Get Help
If you think someone has been poisoned, call the emergency number right away. Do not wait for the child to look or feel sick. The poison center will tell you what to do to help the child. Make sure you know the poison center’s telephone number. Keep a card or sticker with the poison center’s telephone number, carry it with you on your babysitting jobs and save the number in your cell phone.
Poison Prevention Week
To keep your car safe:
*
Think of your vehicle as your home on wheels. Apply the same poison prevention tips that work at home to your automobile.
*
Keep automotive products and car cleaner products in their original containers. Don't, for example, put windshield washer fluid in a used plastic water bottle, lest someone accidentally drink it.
*
Keep products locked and out of reach of children. If you don't have a trunk, use a plastic container with a snug top.
*
Give children appropriate toys to play with and not a purse, which can hold pills, caffeine gum, hair spray or other inappropriate products. Same goes for diaper bags.
*
Inspect any packaging you may give a little one to play with on car rides. No plastic bags, for example.
Unintentional Injury Prevention
http://www.cdc.gov/ncipc/duip/duip.htm
The Division of Unintentional Injury Prevention in CDC's Injury Center monitors trends in unintentional injuries in the United States, conducts research to better understand risk factors, and evaluates interventions to prevent these injuries. Research and prevention programs focus on two categories of unintentional injury: motor vehicle-related injuries and home and recreation related injuries.
Unintentional Injury Prevention
The Division of Unintentional Injury Prevention in CDC's Injury Center monitors trends in unintentional injuries in the United States, conducts research to better understand risk factors, and evaluates interventions to prevent these injuries. Research and prevention programs focus on two categories of unintentional injury: motor vehicle-related injuries and home and recreation related injuries.
Podcasts—Unintentional Injury Prevention
Publications
Fact Sheets about Unintentional Injury Topics
Research Updates (Brief summaries of study findings):
* Car Surfing: A Dangerous, Thrill-Seeking Activity
* CDC Recommends Booster Seats for Children
* Child Passengers Killed in Alcohol-Related Crashes Usually Riding with a Drinking Driver
* Community-Based Interventions to Reduce Motor Vehicle-Related Injuries
* Effectiveness of Designated Driver Promotion Programs to Reduce Alcohol-Impaired Driving is Unknown
* Feasibility of Expanding NEISS to Monitor Nonfatal Injuries Treated in US Emergency Departments
* Graduated Driver Licensing Reduces Risk of Young Driver Crashes
* Implementing impaired driving countermeasures: Putting research into action
* Motor Vehicle-Related Injuries Among Older Adults: A Growing Public Health Concern
* Primary Enforcement Laws Reach Groups Least Likely to Use Safety Belts
* Reducing Motor Vehicle Crashes Among Young Drivers
* Research Update: Lessons from CDC’s Smoke Alarm Installation and Fire Safety Education Program
* School-based Programs Reduce Riding with Alcohol-impaired Drivers
* Sobriety Checkpoints Are Effective in Reducing Alcohol-Related Crashes
* Stronger State DUI Prevention Activities May Reduce Alcohol-Impaired Driving
* The Choking Game: CDC’s Findings on a Risky Youth Behavior
Publications Available Online or for Order
* Activity Report 2004: CDC’s Unintentional Injury Prevention Program
* Activity Report 2001: CDC’s Unintentional Injury Prevention Program
* Atlas of Injury Mortality Among American Indian and Alaska Native Children and Youth
* Bicycle Helmet Recommendations
* Check for Safety: A Home Fall Prevention Checklist for Older Adults - included in tool kit (also available in Spanish).
* Demonstrating Your Program's Worth: A Primer on Evaluation for Programs to Prevent Unintentional Injury
* Efforts to Increase Smoke Detector Use in U.S. Households
* Home and Leisure Injuries in the United States: A Compendium of Articles from the Morbidity and Mortality Weekly Report 1985-1999
* Injury Mortality Among American Indian and Alaska Native Children and Youth, 1989–1998
MMWR Article
Fact Sheet
* Major Causes of Unintentional Injuries Among Older Persons
* National Strategies for Advancing Child Pedestrian Safety
* Nonfatal Choking-Related Episodes Among Children --- United States, 2001
* Prevention of Motor Vehicle-Related Injuries: A Compendium of Articles from the Morbidity and Mortality Weekly Report 1985-1996
* U.S. Fall Prevention Programs for Seniors
Selected Programs Using Home Assessment and Modification
* Unpowered Scooter-Related Injuries --- United States, 1998--2000
* What YOU Can Do To Prevent Falls - included in tool kit (also available in Spanish)
Spotlights
* Click It or Ticket
* Child Passenger Safety Week
* Choking Episodes Among Children
* Dog Bite Prevention Week
* Drunk and Drugged Driving Prevention
* Fire Prevention Week
* Fireworks Safety Month
* International Day of Older Persons
* Walk to School Day
* World Day of Remembrance for Road Traffic Victims
* Community-Based Interventions to Reduce Motor Vehicle-Related Injuries
* Safe Boating Week
* Teens Behind the Wheel: Graduated Driver Licensing
* World Health Day 2004
* Links to non-Federal organizations found at this site are provided solely as a service to our users. These links do not constitute an endorsement of these organizations or their programs by CDC or the Federal Government, and none should be inferred. CDC is not responsible for the content of the individual organization Web pages found at these links.
PDF Document Icon Please note: Some of these publications are available for download only as *.pdf files. These files require Adobe Acrobat Reader in order to be viewed. Please review the information on downloading and using Acrobat Reader software.
Content Source: National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention
Page last modified: October 23, 2008
Page Located on the Web at http://www.cdc.gov/ncipc/duip/duip.htm
Department of Health and Human Services
Additional Information Regarding Disposal of Medications
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5910a8.htm?s_cid=mm5910a8_e
Weekly
March 19, 2010 / 59(10);302
In the report, Adult Use of Prescription Opioid Pain Medications Utah, 2008, in the last paragraph of the Editorial Note (page 156), a reference is made to Food and Drug Administration recommendations for the appropriate disposal of leftover medications from the household if the local community does not have a medication disposal or "take back" program. These guidelines include a list of medications with special labeling directions recommending they be disposed of by flushing down the sink or toilet. This method for disposal is recommended because a number of potent opioids are included on the list, and these medications can be harmful, even fatal, if taken accidentally. The guidelines and list are available at http://www.fda.gov/drugs/resourcesforyou/consumers/buyingusingmedicinesafely/ensuringsafeuseofmedicine/safedisposalofmedicines/ucm186187.htmExternal Web Site Icon.
Disposal by Flushing of Certain Unused Medicines: What You Should Know
* Overview
* Frequently Asked Questions
* List of Medicines Recommended for Disposal by Flushing
Medicines play an important role in treating certain conditions and diseases, but they must be taken with care. Unused portions of these medicines must be disposed of properly to avoid harm. Almost all medicines can be thrown away in the household trash after mixing them with some unpalatable substance (e.g., coffee grounds) and sealing them in a container.
However, certain medicines may be especially harmful and, in some cases, fatal in a single dose if they are used by someone other than the person the medicine was prescribed for. For this reason, a few medicines have special disposal directions that indicate they should be flushed down the sink or toilet after the medicine is no longer needed. If you dispose of these medicines down the sink or toilet, they cannot be accidently used by children, pets, or anybody else.
You may have also received disposal directions for these medicines when you picked up your prescription. If your medicine is on this list, and you did not receive information on disposal with your prescription, you can find directions on how to dispose of the medicines at DailyMed1. After you search on the drug name, the disposal information for these medicines can be found in one of the following sections of the prescribing information:
* Information for Patients and Caregivers
* Patient Information
* Patient Counseling Information
* Safety and Handling Instructions
* Medication Guide
It is important to note that disposal by flushing is not recommended for the vast majority of medicines. Unused or expired medicines that do not have flushing directions in the label can be disposed of safely in the household trash by:
1. Mixing them with something that will hide the medicine or make it unappealing, such as kitty litter or used coffee grounds.
2. Placing the mixture in a container such as a sealed plastic bag.
3. Throwing the container in your household trash.
Below is some additional information about the disposal of medicine that is no longer needed. If you have additional questions about disposing of your medicine, please contact us at 1-888-INFO-FDA (1-888-463-6332).
Frequently Asked Questions
Why do the medications on the list have flushing directions for disposal?
The medicines on this list of medicines recommended for disposal by flushing are safe and effective when used as prescribed, but they could be especially harmful to a child, pet, or anyone else if taken accidentally. Some of the possible harmful effects include breathing difficulties or heart problems, possibly leading to death. For these reasons, FDA advises that flushing these medicines down the sink or toilet is currently the best way to immediately and permanently remove the risk of harm from the home.
FDA continues to work with and encourage the manufacturers of these medicines to develop alternative, safe disposal systems.
How should you dispose of medicines not found on the list?
Do not flush all medicines down the toilet. The FDA recommends that most medicines be disposed of in the household trash after mixing them with some unpalatable substance (e.g., coffee grounds) and sealing them in a container. Unused portions of medicines must be disposed of properly to avoid harm.
Drug take-back programs for disposal can be another good way to remove unwanted or expired medicines from the home and reduce the chance that someone may accidentally take the medicine. Contact your city or county government's household trash and recycling service to see if there is a take-back program in your community and if there are any rules about which medicines can be taken back. You can also talk to your pharmacist to see if he or she knows of other medicine disposal programs in your area.
Does flushing the medicines on the list down the toilet or sink drain pose a risk to human health and the environment?
We are aware of recent reports that have noted trace amounts of medicines in the water system. The majority of medicines found in the water system are a result of the body’s natural routes of drug elimination (in urine or feces). Scientists, to date, have found no evidence of harmful effects to human health from medicines in the environment.
Disposal of these select, few medicines by flushing contributes only a small fraction of the total amount medicine found in the water. FDA believes that any potential risk to people and the environment from flushing this small, select list of medicines is outweighed by the real possibility of life-threatening risks from accidental ingestion of these medicines.
MEDICINES RECOMMENDED FOR DISPOSAL BY FLUSHING
This list from FDA tells you what unused or expired medicines you should flush down the sink or toilet to help prevent danger to people and pets in the home. Flushing these medicines will get rid of them right away and help keep your family and pets safe.
FDA continually evaluates medicines for safety risks and will update the list as needed.
Medicine Active Ingredient
Actiq, oral transmucosal lozenge Fentanyl Citrate
Avinza, capsules (extended release) Morphine Sulfate
Daytrana, transdermal patch system Methylphenidate
Demerol, tablets * Meperidine Hydrochloride
Demerol, oral solution * Meperidine Hydrochloride
Diastat/Diastat AcuDial, rectal gel Diazepam
Dilaudid, tablets * Hydromorphone Hydrochloride
Dilaudid, oral liquid * Hydromorphone Hydrochloride
Dolophine Hydrochloride, tablets * Methadone Hydrochloride
Duragesic, patch (extended release) * Fentanyl
Embeda, capsules (extended release) Morphine Sulfate; Naltrexone Hydrochloride
Fentora, tablets (buccal) Fentanyl Citrate
Kadian, capsules (extended release) Morphine Sulfate
Methadone Hydrochloride, oral solution * Methadone Hydrochloride
Methadose, tablets * Methadone Hydrochloride
Morphine Sulfate, tablets (immediate release) * Morphine Sulfate
Morphine Sulfate, oral solution * Morphine Sulfate
MS Contin, tablets (extended release) * Morphine Sulfate
Onsolis, soluble film (buccal) Fentanyl Citrate
Opana, tablets (immediate release) Oxymorphone Hydrochloride
Opana ER, tablets (extended release) Oxymorphone Hydrochloride
Oramorph SR, tablets (sustained release) Morphine Sulfate
Oxycontin, tablets (extended release) * Oxycodone Hydrochloride
Percocet, tablets * Acetaminophen; Oxycodone Hydrochloride
Percodan, tablets * Aspirin; Oxycodone Hydrochloride
Xyrem, oral solution Sodium Oxybate
*These medicines have generic versions available or are only available in generic formulations.
List revised: August 2009
For specific drug product labeling information, go to DailyMed2 or Drugs@FDA3.
-
Additional Resources
* New FDA Web Page Lists Disposal Instructions for Select Medicines4
* How to Dispose of Unused Medicines5
* Medication Disposal: Questions and Answers6
* Federal Guidelines for Proper Disposal of Drugs7
* Environmental Protection Agency8
-
Subscribe to:
Post Comments (Atom)
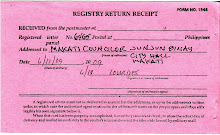
image of registry return receipt of letter addressed to Makati councilor J. J. Binay

No comments:
Post a Comment