web site with useful, free information:
Bartleby Reference
Bartleby.com
Tips for people who eat out
http://www.consumeraffairs.iocom/news04/2007/10/healthy_restaurants.html
Tips for users of notebook computers
http://www.pcworld.com/article/156028/article.html?tk=nl_mcxblg
Mass Casualty Event Preparedness and Response
http://emergency.cdc.gov/masscasualties/
Info for the General Public
Preparing for a Terrorist Bombing: A Common Sense Approach
Although terrorists use a variety of methods to inflict harm and create fear, bombs are used most frequently. According to the U. S. Federal Bureau of Investigation, bombings accounted for nearly 70 percent of all terrorist attacks in the U.S. and its territories between 1980 and 20011. This document focuses on common sense principles that will be useful in a bombing event.
What can I do now?
CDC and the American Red Cross encourage every organization, family and individual to take time to prepare for an emergency or disaster. These steps can help you get started:
* Know your work, school and community disaster plans. If you are not familiar with the plans, contact your supervisor, school administrators, or your local fire department for information.
* Identify an alternative hospital. Hospitals closest to the event are always the busiest.
* Visit http://www.redcross.org/preparedness. The site provides guidance on creating a disaster plan and steps you can take now to protect yourself and your loved ones.
What should I do if I think someone is going to set off a bomb?
At Home At Work At School In Public
Leave the area immediately. Follow existing evacuation guidelines.
Call 9-1-1. Tell the operator what you saw or know (suspicious persons, packages, or vehicles). Call 9-1-1. Tell the operator what you saw or know (suspicious persons, packages, or vehicles).
Follow directions from people in authority (police, fire, EMS, or military personnel, or from workplace supervisors. or from school administrators, or from commumity leaders).
What should I do during a terrorist bombing?
If you are in a bombing event:
* Leave the area immediately.
* Avoid crowds. Crowds of people may be targeted for a second attack.
* Avoid unattended cars and trucks. Unattended cars and trucks may contain explosives.
* Stay away from damaged buildings to avoid falling glass and bricks. Move at least 10 blocks or 200 yards away from damaged buildings.
* Follow directions from people in authority (police, fire, EMS, or military personnel, or from school or workplace supervisors).
* Call 9-1-1 once you are in a safe area, but only if police, fire, or EMS has not arrived.
* Help others who are hurt or need assistance to leave the area if you are able. If you see someone who is seriously injured, seek help. Do not try to manage the situation alone.
What should I do after the bombing?
When the explosion is over:
* Follow your family, job, or school emergency disaster plan for leaving and staying away from the scene of the event. Remember, returning to the scene will increase the risk of danger for rescue workers and you.
* Avoid crowds. Crowds of people may be targeted for a second attack.
* Avoid unattended cars and trucks. Unattended cars and trucks may contain explosives.
* Stay away from damaged buildings to avoid falling glass and bricks. Move at least 10 blocks or 200 yards away from damaged buildings.
* Follow directions from people in authority (police, fire, EMS, or military personnel, or from school or workplace supervisors).
* Call 9-1-1 once you are in a safe area, but only if police, fire, or EMS has not arrived to help injured people.
* Help others who are hurt or need assistance to leave the area if you are able. If you see someone who is seriously injured, seek help. Do not try to manage the situation alone.
* Listen to your radio or television for news and instructions.
What if rescue workers are not available to transport me or other injured persons?
9-1-1 services (police, fire, EMS and ambulance) might be delayed indefinitely following a terrorist event, therefore:
* Always have a back-up plan for transportation.
* Follow advice from your local public safety offices (local health department, local emergency management offices, fire and police departments and reliable news sources).
When should I go to the hospital or clinic?
Seek medical attention if you have any of the following problems:
* Excessive bleeding
* Trouble breathing
* Persistent cough
* Trouble walking or using an arm or leg
* Stomach, back or chest pains
* Headache
* Blurred vision or burning eyes
* Dry mouth
* Vomiting or diarrhea
* Rash or burning skin
* Hearing problems
* Injuries that increase in pain, redness or swelling
* Injuries that do not improve after 24 to 48 hours
Help others who are hurt or need assistance to leave the area, if you are able.If you see someone who is seriously injured, seek help. Do not try to manage the situation alone.
Where should I go for care?
Go to a hospital or clinic away from the event if you can. Most victims will go to the nearest hospital. Hospitals away from the event will be less busy.
What can I expect at the hospital?
* Long waits. To avoid long waits, choose a hospital farther away from the event. While this might increase your travel time, you might receive care sooner.
* Triage. Following a terrorist attack or other disasters, injuries are generally treated on a “worst first” basis, called “triage.” Triage is not “first come, first served”. If your injuries are not immediately life threatening, others might be treated before you. The goal of triage is to save as many lives as possible.
* Limited information. In a large-scale emergency such as a terrorist attack, police, fire, EMS, and even hospitals and clinics cannot track every individual by name. Keep in mind that it may be difficult for hospitals to provide information about loved ones following a terrorist attack. Be patient as you seek information.
For more information about how to prepare for a terrorist bombing and other disasters, click on the related links:
* American Red Cross, “Terrorism—Preparing for the Unexpected.” http://www.redcross.org/services/disaster/0,1082,0_589_,00.html.
* Federal Emergency Management Agency (FEMA), http://www.fema.gov.
* Mass casualties and injuries from terrorism, CDC’s Emergency Preparedness and Response Website. http://emergency.cdc.gov.
* United States Department of Homeland Security, http://www.ready.gov.
1. U.S. Department of Justice, Federal Bureau of Investigation, Terrorism 1980-2001. www.fbi.gov/publications/terror/terror2000_2001.htm
Coping With a Traumatic Event:
Information for the Public (see also Information for Health Professionals)
HIGHLIGHTS
* Traumatic events often cause feelings of fear, grief and depression.
* There are many things you can do to cope with traumatic events, including talking to family, friends, and clergy for support.
* Let your child know that it is okay to feel upset when something bad or scary happens.
* You may need to consider seeking professional help if your feelings affect your relationship with your family and friends, or affect your job.
What Is a Traumatic Event?
Most everyone has been through a stressful event in his or her life. When the event, or series of events, causes a lot of stress, it is called a traumatic event. Traumatic events are marked by a sense of horror, helplessness, serious injury, or the threat of serious injury or death. Traumatic events affect survivors, rescue workers, and the friends and relatives of victims who have been involved. They may also have an impact on people who have seen the event either firsthand or on television.
What Are Some Common Responses?
A person’s response to a traumatic event may vary. Responses include feelings of fear, grief and depression. Physical and behavioral responses include nausea, dizziness, and changes in appetite and sleep pattern as well as withdrawal from daily activities. Responses to trauma can last for weeks to months before people start to feel normal again.
Most people report feeling better within three months after a traumatic event. If the problems become worse or last longer than one month after the event, the person may be suffering from post-traumatic stress disorder (PTSD).
What Is PTSD?
Post-traumatic stress disorder (PTSD) is an intense physical and emotional response to thoughts and reminders of the event that last for many weeks or months after the traumatic event. The symptoms of PTSD fall into three broad types: re-living, avoidance and increased arousal.
* Symptoms of re-living include flashbacks, nightmares, and extreme emotional and physical reactions to reminders of the event. Emotional reactions can include feeling guilty, extreme fear of harm, and numbing of emotions. Physical reactions can include uncontrollable shaking, chills or heart palpitations, and tension headaches.
* Symptoms of avoidance include staying away from activities, places, thoughts, or feelings related to the trauma or feeling detached or estranged from others.
* Symptoms of increased arousal include being overly alert or easily startled, difficulty sleeping, irritability or outbursts of anger, and lack of concentration.
Other symptoms linked with PTSD include: panic attacks, depression, suicidal thought and feelings, drug abuse, feelings of being estranged and isolated, and not being able to complete daily tasks.
What Can You Do for Yourself?
There are many things you can do to cope with traumatic events.
* Understand that your symptoms may be normal, especially right after the trauma.
* Keep to your usual routine.
* Take the time to resolve day-to-day conflicts so they do not add to your stress.
* Do not shy away from situations, people and places that remind you of the trauma.
* Find ways to relax and be kind to yourself.
* Turn to family, friends, and clergy person for support, and talk about your experiences and feelings with them.
* Participate in leisure and recreational activities.
* Recognize that you cannot control everything.
* Recognize the need for trained help, and call a local mental health center.
What Can You Do for Your Child?
* Let your child know that it is okay to feel upset when something bad or scary happens.
* Encourage your child to express feelings and thoughts, without making judgments.
* Return to daily routines.
When Should You Contact Your Doctor or Mental Health Professional?
About half of those with PTSD recover within three months without treatment. Sometimes symptoms do not go away on their own or they last for more than three months. This may happen because of the severity of the event, direct exposure to the traumatic event, seriousness of the threat to life, the number of times an event happened, a history of past trauma, and psychological problems before the event.
You may need to consider seeking professional help if your symptoms affect your relationship with your family and friends, or affect your job. If you suspect that you or someone you know has PTSD, talk with a health care provider or call your local mental health clinic.
Emergency Wound Care After a Natural Disaster
(NOTE: Health professionals should see Emergency Wound Management for Healthcare Professionals.)
The risk for injury during and after a hurricane and other natural disasters is high. Prompt first aid can help heal small wounds and prevent infection. Tetanus is a potential health threat for persons who have open wounds.
Seek medical attention as soon as possible if:
* There is a foreign object embedded in the wound;
* The wound is at special risk of infection (such as a dog bite or a puncture by a dirty object);
* An old wound shows signs of becoming infected (increased pain and soreness, swelling, redness, draining, or you develop a fever).
How to Care for Minor Wounds
* Wash your hands thoroughly with soap and clean water if possible.
* Avoid touching the wound with your fingers while treating it (if possible, use disposable, latex gloves).
* Remove obstructive jewelry and clothing from the injured body part.
* Apply direct pressure to any bleeding wound to control bleeding.
* Clean the wound after bleeding has stopped.
o Examine wounds for dirt and foreign objects.
o Gently flood the wound with bottled water or clean running water (if available, saline solution is preferred).
o Gently clean around the wound with soap and clean water.
o Pat dry and apply an adhesive bandage or dry clean cloth.
* Leave unclean wounds, bites, and punctures open. Wounds that are not cleaned correctly can trap bacteria and result in infection.
* Provide pain relievers when possible.
Other Considerations
* Expect a variety of infection types from wounds exposed to standing water, sea life, and ocean water.
* Wounds in contact with soil and sand can become infected.
* Puncture wounds can carry bits of clothing and dirt into wounds and result in infection.
* Crush injuries are more likely to become infected than wounds from cuts.
* Take steps to prevent tetanus
If you have wounds, you should be evaluated for a tetanus immunization. If you receive a puncture wound or a wound contaminated with feces, soil, or saliva, have a health care professional determine whether a tetanus booster is necessary based on individual records.
References
Krohmer, J.R., Rapp M.T. & American College of Emergency Physicians.(2001). First aid manual: A comprehensive guide to treating emergency victims of all ages in any situation. (3 rd ed.) New York : Dorling Kindersley Limited.
Tintinalli, J.E., Kelen, G.D., Stapczynski, J.S., & American College of Emergency Physicians. (2004). Emergency medicine: A comprehensive guide. (6th ed.) New York : McGraw-Hill.
Injuries and Mass Casualty Events:
Information for the Public (see also Information for Health Professionals)
If you are injured or think you are injured, seek medical attention right away. Injuries that occur during a mass casualty event are at high risk for infection and other long lasting health effects.
What Injuries Occur Most Often?
The most severe injuries in mass casualty events are fractures, burns, lacerations, and crush injuries. However, the most common injuries are eye injuries, sprains, strains, minor wounds, and ear damage.
Why Do These Injuries Occur in Mass Casualty Events?
* Eye injuries and irritation can occur from excess particles (such as soot, dirt, powder, paint chips), fumes or smoke present in the air after a disaster event. More serious eye problems can result from metal or glass fragments that enter the eye at a high speed.
* Sprains and strains are common in these situations and can occur as people escape the scene, fall, are thrown or pushed down by a force, or carry others who are in need of assistance.
* Minor wounds can be caused by flying debris and falling on or scraping against sharp objects.
* Eardrum damage can occur from a foreign body entering the ear, a blow or jolt to the head, or an extreme and sudden noise (i.e. explosion) all of which are likely in a mass casualty event.
How Do Mass Casualty Events Affect My Health?
It is normal for people to suffer emotional and physical stress after a mass casualty event, even if they are not at or near the scene. This additional stress can make existing health conditions worse (for example, diabetes) or trigger a new health problem (for example, heart attack, depression). If a mass casualty event occurs, try to take care of yourself by:
* Maintaining healthy eating, exercise, and sleeping habits;
* Continuing to take your medicine as prescribed by your physician;
* Keeping with your daily routine;
* Talking to people about your feelings and concerns.
What Should I Do If I Have a Health Problem?
Seek medical attention immediately. It is important to see a doctor for injuries and other health problems that arise or worsen after a mass casualty event. Proper medical attention can help prevent complications and long-lasting health effects.
Listen to your local news to identify which hospitals or clinics are open. In mass casualty events, certain hospitals may be closed or only open to certain kinds of patients. However, many other hospitals and clinics, especially those outside the immediate area of the event, will be available to see patients with injuries and other health problems. If you are having a health problem, seek medical care. Do not delay because of a mass casualty event.
For More Information
* Visit the website of your state health department.
* Visit the website of CDC's Injury Center for injury information and resources.
Brain Injuries and Mass Casualty Events:
Information for the Public (see also Information for Clinicians)
Traumatic brain injuries can occur during mass casualty events. If you think you or someone you know has a brain injury, contact your health care provider.
What is a traumatic Brain Injury?
A traumatic brain injury (TBI) is defined as a blow or jolt to the head or a penetrating head injury that disrupts the normal function of the brain.. Not all blows or jolts to the head result in a TBI. The severity of such an injury may range from “mild,” that is, a brief change in mental status or consciousness to “severe,” that is, an extended period of unconsciousness or amnesia after the injury. A TBI can result in short or long-term problems with an individual’s ability to function independently, or changes that affect thinking, memory, sensation, language, and emotions.
Why Are TBIs a Problem in Mass Casualty Events?
In mass casualty events, such as the World Trade Center attack or the Oklahoma City bombing, TBIs were caused by flying debris or by a person falling and hitting their head. A blast from an explosion can also cause a TBI even when there is no direct contact with an object.
What Are Some Common Signs and Symptoms of a TBI?
The signs and symptoms of a TBI can be subtle. Symptoms of a TBI may not appear until days or weeks following the injury or may even be missed as people may look fine even though they may act or feel differently. The following are some common signs and symptoms of a TBI:
* Headaches or neck pain that do not go away;
* Difficulty remembering, concentrating, or making decisions;
* Slowness in thinking, speaking, acting, or reading;
* Getting lost or easily confused;
* Feeling tired all of the time, having no energy or motivation;
* Mood changes (feeling sad or angry for no reason);
* Changes in sleep patterns (sleeping a lot more or having a hard time sleeping);
* Light-headedness, dizziness, or loss of balance;
* Urge to vomit (nausea);
* Increased sensitivity to lights, sounds, or distractions;
* Blurred vision or eyes that tire easily;
* Loss of sense of smell or taste; and
* Ringing in the ears.
What Can You Do to Get Help?
If you think you or someone you know has a TBI, contact your health care provider. Your health care provider can refer you to a neurologist, neuropsychologist, neurosurgeon, or specialist in rehabilitation (such as a speech pathologist). Getting help soon after the injury by trained specialists may speed your recovery.
For More Information, Contact:
The Brain Injury Association of America (BIAA)
* Call the toll-free help line at 1-800-444-6443 for help in English or Spanish
* Visit the website at www.biausa.org
The Defense and Veterans Brain Injury Center (DVBIC)
* Call Toll Free for information 1-800-870-9244
* Visit the website at www.dvbic.org
The Centers for Disease Control and Prevention (CDC)
* Learn about CDC’s TBI-related activities and products online at: http://www.cdc.gov/node.do?id=0900f3ec8000dbdc.
* Download a free copy of CDC’s “ Facts about traumatic Brain Injury” fact sheet.
* Download or order the free brochure, Facts about Concussion and Brain Injury, (in English and Spanish) online at: www.cdc.gov/ncipc/tbi/default.htm.
Mass Casualties: Burns
Mass casualties and disasters such as explosions and fires can cause a variety of serious injuries, including burns. These can include thermal burns, which are caused by contact with flames, hot liquids, hot surfaces, and other sources of high heat as well as chemical burns and electrical burns. It is vital that people understand how to behave safely in mass casualty and fire situations, as well as comprehend basic principles of first aid for burn victims. For burns, immediate care can be lifesaving.
Note: Most victims of fires die from smoke or toxic gases, not from burns (Hall 2001). This guideline covers burn injuries.
Background Information
* On average in the United States in 2004, someone died in a fire every 135 minutes, and someone was injured every 30 minutes (Karter 2005).
* Each year in the United States, 1.1 million burn injuries require medical attention (American Burn Association, 2002).
o Approximately 50,000 burn injuries require hospitalization;
o Approximately 20,000 are major burns involving at least 25 percent of the total body surface;
o Approximately 4,500 of these people die.
* Up to 10,000 people in the United States die every year of burn-related infections.
* Only 60 percent of Americans have an escape plan, and of those, only 25 percent have practiced it (NFPA, 1999).
* Smoke alarms cut your chances of dying in a fire in half (NFPA, 1999).
Escape Information
Safeguard Your Home
* Install smoke alarms on each floor of your home. One alarm must be outside a bedroom where you sleep.
* Change batteries in smoke alarms at least once a year. (Never borrow smoke alarm batteries for other purposes).
* Keep emergency phone numbers and other pertinent information posted close to your telephone.
* Draw a floor plan and find two exits from each room. Windows can serve as emergency exits.
* Practice getting out of the house through the various exits.
* Designate a meeting place at a safe distance outside the home.
* Respond to every alarm as if it were a real fire.
* Call the fire department after escaping. Tell them your address and do not hang up until you are told to do so. Let them know if anyone is trapped inside.
* Never go back into a burning building to look for missing people, pets, property, etc. Wait for firefighters.
Hotel and Workplace Fire Safety
* Become familiar with exits and posted evacuation plans each time you enter a building.
* Learn the location of all building exits. You may have to find your way out in the dark.
* Ensure that fire exits are unlocked and clear of debris.
* All buildings, whether homes, workplaces or hotels, should have working smoke alarm systems. Make sure you know what the alarm sounds like.
* Respond to every alarm as if it were a real fire. If you hear an alarm, leave immediately and close doors behind you as you go.
* Establish an outside meeting place where everyone can meet after they have escaped.
* Call the fire department after escaping. Tell them your address and do not hang up until you are told to do so. Let them know if anyone is trapped inside.
* Never go back into a burning building to look for missing people, pets, property, etc. Wait for firefighters.
If You Are Trapped in a Burning Building
* Smoke rises, so crawl low to the ground where the air will be cleanest.
* Get out quickly if it is safe to leave. Cover your nose and mouth with a cloth (moist if possible).
* Test doorknobs and spaces around doors with the back of your hand. If the door is warm, try another escape route. If it is cool, open it slowly. Check to make sure your escape path is clear of fire and smoke.
* Use the stairs. Never use an elevator during a fire.
* Call the fire department for assistance if you are trapped. If you cannot get to a phone, yell for help out the window. Wave or hang a sheet or other large object to attract attention.
* Close as many doors as possible between yourself and the fire. Seal all doors and vents between you and the fire with rags, towels, or sheets. Open windows slightly at the top and bottom, but close them if smoke comes in.
First Aid
What you do to treat a burn in the first few minutes after it occurs can make a huge difference in the severity of the injury.
Immediate Treatment for Burn Victims
1. “Stop, Drop, and Roll” to smother flames.
2. Remove all burned clothing. If clothing adheres to the skin, cut or tear around burned area.
3. Remove all jewelry, belts, tight clothing, etc., from over the burned areas and from around the victim’s neck. This is very important; burned areas swell immediately.
Types of Burns
First-Degree Burns
First-degree burns involve the top layer of skin. Sunburn is a first-degree burn.
Signs:
* Red
* Painful to touch
* Skin will show mild swelling
Treatment:
* Apply cool, wet compresses, or immerse in cool, fresh water. Continue until pain subsides.
* Cover the burn with a sterile, non-adhesive bandage or clean cloth.
* Do not apply ointments or butter to burn; these may cause infection.
* Over-the-counter pain medications may be used to help relieve pain and reduce inflammation.
* First degree burns usually heal without further treatment. However, if a first-degree burn covers a large area of the body, or the victim is an infant or elderly, seek emergency medical attention.
Second-Degree Burns
Second-degree burns involve the first two layers of skin.
Signs:
* Deep reddening of the skin
* Pain
* Blisters
* Glossy appearance from leaking fluid
* Possible loss of some skin
Treatment:
* Immerse in fresh, cool water, or apply cool compresses. Continue for 10 to 15 minutes.
* Dry with clean cloth and cover with sterile gauze.
* Do not break blisters.
* Do not apply ointments or butter to burns; these may cause infection
* Elevate burned arms or legs.
* Take steps to prevent shock: lay the victim flat, elevate the feet about 12 inches, and cover the victim with a coat or blanket. Do not place the victim in the shock position if a head, neck, back, or leg injury is suspected, or if it makes the victim uncomfortable.
* Further medical treatment is required. Do not attempt to treat serious burns unless you are a trained health professional.
Third-Degree Burns
A third-degree burn penetrates the entire thickness of the skin and permanently destroys tissue.
Signs:
* Loss of skin layers
* Often painless. (Pain may be caused by patches of first- and second-degree burns which often surround third-degree burns).
* Skin is dry and leathery
* Skin may appear charred or have patches which appear white, brown or black
Treatment:
* Cover burn lightly with sterile gauze or clean cloth. (Do not use material that can leave lint on the burn).
* Do not apply ointments or butter to burns; these may cause infection
* Take steps to prevent shock: lay the victim flat, elevate the feet about 12 inches.
* Have person sit up if face is burned. Watch closely for possible breathing problems.
* Elevate burned area higher than the victim’s head when possible. Keep person warm and comfortable, and watch for signs of shock.
* Do not place a pillow under the victim’s head if the person is lying down and there is an airway burn. This can close the airway.
* Immediate medical attention is required. Do not attempt to treat serious burns unless you are a trained health professional.
References
Ahrens M. (2001) The U.S. fire problem overview report: Leading causes and other patterns and trends. Quincy (MA): National Fire Protection Association.
American Burn Associations (2002). Burn Incidence Fact Sheet.
Burn Foundation (2002) Travel Safe Guide - Surviving a Hotel Fire.
CDC, National Center for Health Statistics (NCHS). (1998) National vital statistics system. Hyattsville (MD): U.S. Department of Health and Human Services, CDC, National Center for Health Statistics.
Gibran NS, Heimbach DM. (2000) Current status of burn wound pathophysiology. Clinical Plastic Surgery; 27 (1): 11-22.
Gueugniaud PY, et al. (2000) Current advances in the initial management of major thermal burns. Intensive Care Med; 26 (7): 848-56.
Hall JR. (2001) Burns, toxic gases, and other hazards associated with fires: Deaths and injuries in fire and non-fire situations. Quincy (MA): National Fire Protection Association, Fire Analysis and Research Division.
Hilton G. (2001) Emergency. Thermal burns. AJ7N, American Journal of Nursing. 101(11):32-4.
Istre GR, McCoy MA, Osbom L, Bamard JJ, Bolton A. (2001) Deaths and injuries from house fires. New England Journal of Medicine; 344:1911—16.
Karter MJ. (2005) Fire loss in the United States during 2004. Quincy (MA): National Fire Protection Association, Fire Analysis and Research Division.
National Fire Protection Association (1999) NFPA National Fire Escape Survey, Quincy (MA).
Parker DJ, Sklar DP, Tandberg D, Hauswald M, Zumwalt RE. (1993) Fire fatalities among New Mexico children. Annals of Emergency Medicine; 22(3):5 17—22.
Yowler CJ, Fratianne RB. (2000) Current status of burn resuscitation. Clinical Plastic Surgery; 27 (1): 1-10.
Information from U.S.FDA regarding INNOHEP
[PDF] IMPORTANT INNOHEP (tinzaparin sodium injection) SAFETY INFORMATION ...
Page 1. Celgene Corporation 86 Morris Avenue Summit, New Jersey 07901 Tel
908-673-9000 Fax 908-673-9001 IMPORTANT INNOHEP ® (tinzaparin ...
www.fda.gov/medwatch/safety/2008/Celgene_Innohep_DHCP_Letter.pdf - 12-31-2008 - Text Version
www.fda.gov/cder/whatsnew.htm - 12-31-2008 - Cached
Faulty Instructions Prompt Recall of Electrical Wiring How-to-Books by The Taunton Press; Shock Hazard to Consumers
http://www.cpsc.gov/cpscpub/prerel/prhtml09/09078.html
Subscribe to:
Post Comments (Atom)
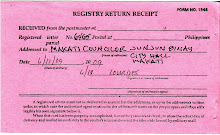
image of registry return receipt of letter addressed to Makati councilor J. J. Binay

No comments:
Post a Comment